This 3-part series was originally published in the Auburn Journal in three consecutive issues on August 17, 18, 20. It is presented here in its entirety.
Part 1: Away We Go
I didn’t even know this neighborhood existed in Auburn, and I’m from here. Million-dollar homes nestle up beside multimillion-dollar homes, each offering the same stunning view, from similarly stunning decks, of the American River Confluence. From where I sit, with the rest of Auburn beneath us, it’s easy to get lost in thought. For a brief moment, I forget the real reason I’m here.
The gram of heroin in my hand snaps me back to reality with a force that I wasn’t expecting.
“If you buy in bulk, it’s cheaper,” my host states flatly, eyes darting around as if he’s half-expecting a SWAT team to be trailing me. “$800 an ounce if you know who to call.” He smirks. “I know who to call.”
After a brief lesson in weights, measures and the almighty dollar, it’s time to get down to business. My host — we’ll call him Kevin — knows that to grant interviews in his line of work is not only dangerous but potentially deadly. In this particular business, talking too much is a failing business model; his reluctance is understandable. Then, without notice, he breaks character, saying what would be perhaps the truest and most real thing I’d hear throughout my month of research for this article:
“This drug is the devil,” he states matter-of-factly. “If me talking to you helps stop what is happening in Auburn right now, then I’ll do it. Because it’s getting bad.”

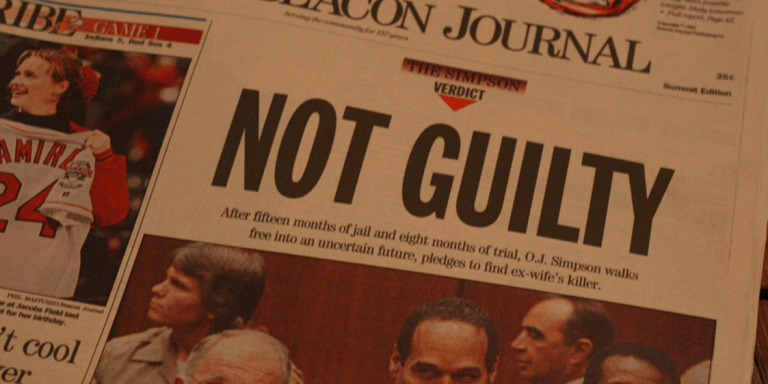
Photo by Jason Smith
As is the case with most addicts, Kevin’s descent into the drug world began innocently enough.
“It started with pills,” he explains, a little something to change the way he felt, be it at a party to have fun or alone to relax. “Vicodin, Norco, Percocet… they were everywhere.” Climbing that narcotic ladder one rung at a time—Roxies, Opana, Fentanyl—eventually brought him to OxyContin.
“OxyContin was like the initiation for a heroin addict,” he says. The actual addiction to OxyContin came on slowly: Once a week, then every few days. Every other day, then only at night. Only to wake up, then only to sleep. Suddenly, the line between wanting the drug and needing the drug became blurred. Using throughout the day was now the only way to keep from getting sick, and it was then that he learned you could take a razor blade to the pill and snort the drug. Or better yet, smoke it.
“In 2006, you could get one 80-milligram pill for $5,” he says, almost longingly. “By 2012, it cost $80 for the same pill.” Using that much Oxy was not economically feasible, meaning heroin was suddenly a viable alternative. It was the same high, but much more affordable.
If switching from OxyContin to heroin was a financial decision, becoming a dealer was a business decision.
Inserting himself between the supply coming up from Sacramento and the increasing demand amongst the 18- to 30-year-old crowd in Auburn, he has been able to finance his own daily use without going broke, something at which very few addicts are ever successful.
“The heroin only touches about four people’s hands between the cartel and me,” he says. If one believes the rule of supply and demand, based on the price alone, demand in the Auburn area began to skyrocket. “I’d go down to San Diego, and they’d be talking about some place up north called Auburn where you could go to make quick money. It was crazy. It happened so fast.”
Auburn’s increase in heroin use since 2006 would mirror what was happening throughout the rest of the country. The Centers for Disease Control and Prevention found that from 2007 to 2011, heroin use more than doubled. A study by the Journal of the American Medical Association, led by Washington University psychiatrist Thomas Cicero, found that 75 percent of those who began using heroin in the 2000s started by abusing prescription drugs. Of those, 94 percent reported to have switched because the prescription drugs got both more expensive and harder to find.
This coincided with the Drug Enforcement Agency’s pressuring of doctors to use more discretion in prescribing narcotics.
In 2010, Purdue Pharmaceuticals, the maker of OxyContin, changed the makeup of the drug so it would be nearly impossible to snort, smoke, or inject via syringe.
“That changed the whole game, right there, when they changed the OxyContins,” explains Kevin, the dealer. “Nothing was the same after that.”
An enormous void in the narcotic supply was created at the exact moment the demand was at an all-time high — a void that heroin was more than able to fill.
Heroin use by young white people in suburban areas became more prevalent, for the first time in American history, than heroin use in inner cities.
And those suburbs are demographically no different from those in the Sierra foothills.
Kristin Netto, 27 of Placerville, had no idea she was about to live this statistic firsthand when, just to be safe, she tagged along with her husband to his doctor’s appointment after he hurt his back at work. He’d struggled with addiction in the past, and she wanted to be sure his doctor knew this. They described to the doctor her husband’s past struggles, and how they wished to avoid any sort of narcotic medication. To their shock, the doctor wrote a prescription for Norco, a powerful semi-synthetic opioid derived from codeine.
“It’s not a problem if he really needs them,” the doctor said. “It’s only addictive if you take them without pain.”
She tried hiding his pills and dispensing them per the instructions on the bottle, continually counting how many were left, but something was always off. While his behavior became more erratic, she tried her best to convince herself that he hadn’t progressed from using the Norco to something far more sinister.
She wanted to believe him. She really did. His mood swings, the constantly fatigue, the progressive disregard for personal hygiene, his apathy toward the condition of the house, her discovery of disassembled Q-tips in the bathroom, his strange habit of always carrying around a lighter despite not smoking cigarettes — she tried her best to pretend none of this had anything to do with drugs. She even bought his excuse that his random drug test from work that came up positive for heroin was some sort of misunderstanding.
Then came Jan. 16, 2014.
The Placer County Sheriff’s Office called, asking her to come pick up her car and toddler son. When she arrived on scene, an officer looked her in the eyes and asked, “Do you have any idea what your husband’s been doing?”
Not knowing the answer would have been bad enough. Knowing the answer was far worse.
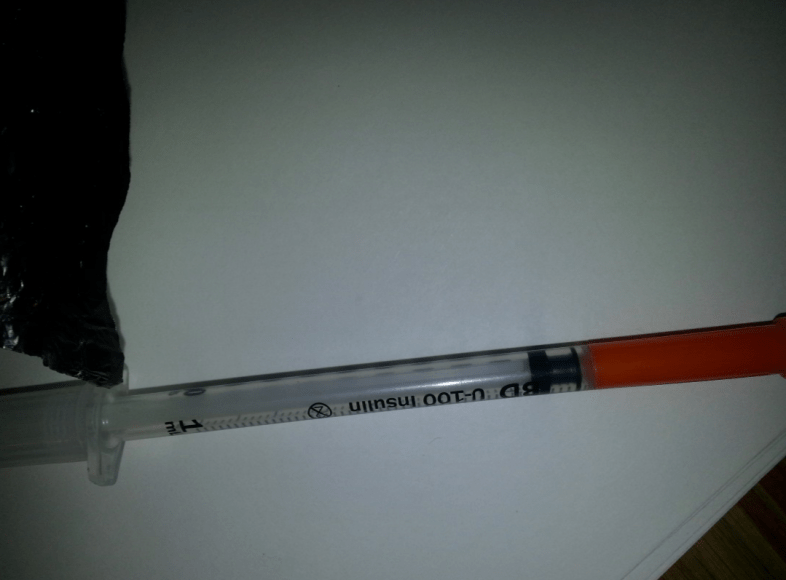
The officer pulled out the syringe, spoon, lighter and small amount of black-tar heroin that had been found in the car. Her husband had already been taken to jail. The baby sat, still screaming, in his car seat.
The disintegration of Kristen’s marriage — and thus, her life — due to heroin addiction took just six months from beginning to end. It squashed the argument that drug abuse is a “victimless” crime.
“I must have called 20 different rehabs to get him into, and each said the same thing: ‘Your husband’s story of back injury to pills to heroin is what we’re hearing every day,’” she says.
It was even less comforting to know she wasn’t alone in what she was going through.
“The amount of people using heroin in Placerville is just crazy,” she says. “Even the deputy that day told me that it’s getting out of control.”
Control is something “Michael,” a 19-year-old from Auburn, thought he could maintain when it came to drug use. A promising young basketball player for both E.V. Cain and Placer High, he began using Norcos in 10th grade for the typical aches and pains that come with being an athlete.
“They made me feel comfortable,” he explains, “and they came from a doctor, so I figured they were all right.”
By 11th grade, “kids you would never expect to do drugs were taking pills,” he says, still sounding surprised. “They were everywhere.” While parents who failed to secure their medications were unwittingly supplying high school campuses with a healthy amount of narcotics, Michael was progressing in his addiction.
The leap from smoking OxyContin to smoking heroin was a short, much more affordable one. The first time he smoked heroin before a high school basketball game, he’d never felt so alive.
“I played great. No anxieties, no pain,” he says. “I loved it.”
Before long, using before a game went from a luxury to a necessity.
“I couldn’t play without it,” he says, shaking his head. “I needed it. I was hooked.” Finding the drug was easy.
“Auburn is bad right now,” he says. “And it’s not like it’s just my group of friends. Rich, poor, white, black — it doesn’t matter. It’s everywhere: Auburn, Colfax, Loomis, Roseville. …” His voice trails off.
Being in the drug game has granted him backstage access to its inner workings. He explains how gangs from Modesto are coming up to Auburn and fronting entire ounces of heroin to dealers, with little doubt that it will sell quickly.
“Auburn has a reputation of being a bunch of little spoiled white kids with money,” he says, half smiling. “If you can come up with $40 a day, you can maintain (your habit) and your parents will never know.”
Twenty-eight days clean, with our interview wrapping up, Michael sits in reflection.
“You know,” he says, “there’s a sick part of me that worries that my helping you with this article will make it harder to find if I go back out.” He pauses. “But this drug is the devil. It’s evil.”
That’s the second time I’ve heard that said about this drug, and it’s starting to weigh on me. Having recently finished an interview for this story in Roseville, I head up the hill toward Auburn, my mind racing. I think back to what the drug dealer, Kevin, said at the end of our interview.
I’d asked him what he thought Auburn would look like in 10 years if we don’t do something about this now. He sat, thinking for a second, and then laughed, not out of humor but rather of incredulity.
“A black hole,” he said, bluntly, eyebrows raised as if that’s the first time he’s realized his role in all of this.
As I pass the “Welcome to Auburn” billboard, my stereo chooses “The End” by the Doors.
“Lost in a Roman wilderness of pain/and all the children are insane/this is the end.”
Part of me can’t help but wonder if Jim Morrison is right.
An entire generation is being destroyed from the inside out. I feel angry. I feel confused. More than anything, I want to know how this has happened.
Part II — Opiates The New Religion of the Masses
Felix Hoffmann knew he was onto something. With the 20th century right around the corner, he spent his nights in his laboratory in Elberfeld, Germany, adding various compounds to morphine in an attempt to dampen its strength. Morphine was decimating a generation of soldiers who had been treated with the drug for war injuries, only to find it nearly impossible to quit once started. Hoffmann’s boss at Bayer Pharmaceutical, maker of Bayer aspirin, was pushing him hard to come up with something, and what he stumbled upon would have a profound effect upon the next two centuries. What he found was considered a miracle drug.
Hoffmann wasn’t the first to discover the drug, but Bayer Pharmaceutical was first to market it. In 1898, Bayer sold the drug over the counter as a miraculous cough suppressant and pain reliever that was a completely non-addictive morphine substitute.
Bayer took the unusual steps of marketing it in German, English, Italian, French and Russian, making the miracle drug one of the first globally marketed medicines in history.
Finally, Bayer promised, a pain reliever that was non habit-forming and safe.
Bayer named it Heroin.
More than a century after its mass introduction by Bayer, heroin remains a societal infection that not only refuses to heal, but insists upon inching its way toward epidemic proportions.
Placer County sheriff’s Deputy Zach Poiesz, a 16-year veteran who spent the past seven years on the Narcotics Task Force, has had a front-row seat for the drug’s evolution over the past decade.
“In Auburn, right now, I could go out tonight and find heroin and paraphernalia,” he says. “It’s that easy.”
Over the past decade, heroin use has doubled, demonstrating the unusual ability to affect every ethnic group and every economic class. It is truly a nondiscriminatory drug.
“When I first started working narcotics, heroin was rare to come across,” explains Poiesz. “Everything changed when Purdue (Pharmaceutical) changed the binder of the OxyContin.”
In order to understand heroin’s dramatic resurgence, it is first necessary to understand the OxyContin abuse that preceded it. Approved by the US Food and Drug Administration in 1995, OxyContin was designed as a high-dose capsule with time release coating, meaning it would need to be taken only once or twice daily for pain management, compared to traditional oxycodone, which is taken every 4-6 hours.
It was soon discovered that if the dissolvable coating were removed from the tablet, the entire dose could be felt at once. It could be smoked. It could be snorted. It could be dissolved in water and shot up intravenously.
…Its sales that year exceeded $1.5 billion.”
When abused, it was essentially heroin in pill form.
From 1996-2000, Purdue Pharmaceutical, the maker of OxyContin, more than doubled its number of pharmaceutical sales representatives, while using sophisticated data collection that tracked which doctors across the country wrote the highest number of narcotics prescriptions. Purdue then targeted those doctors with a barrage of sales reps — sales reps who received bonuses according to how often those particular doctors prescribed OxyContin.
These were the same market representatives upon whom many doctors relied for education about the dangers of the drug.
With this marketing strategy, OxyContin sales mushroomed from $48 million in 1996 to $1.1 billion in 2000.
Like Bayer a century earlier, Purdue downplayed the danger of the drug, reporting that fewer than 1 percent of OxyContin users became addicted — an absurdly optimistic number in hindsight, and even more absurd when compared to national studies at the time. These studies showed an addiction rate of up to 50 percent among people using opiates for long-term care.
In 2007, Purdue Pharmaceutical, along with three executives, pleaded guilty to deliberately downplaying the risk of OxyContin addiction and abuse.
Purdue was fined $634 million.
Its sales that year exceeded $1.5 billion.
It was during this time, according to Deputy Poiesz, that OxyContin began showing up on the streets in abundance.
“The demographic was 16- to 24-year-olds,” says Poiesz, “and we were finding a large majority of them to be under the influence of prescription narcotics. These pills were prescribed so loosely for so long, and parents weren’t locking up the medications. They were everywhere.”
Demand for OxyContin was so high that the street value, according to Poiesz, ranged from $80-$120 for a single 80-milligram pill.
Abuse was so rampant that Purdue Pharmaceutical was pressured to do something about it. In 2010 it responded by introducing a tamper-resistant coating for the tablet, making it nearly impossible to smoke, snort or inject.
In 2012, the New England Journal of Medicine documented an immediate decline in OxyContin abuse as a result of the formula change — and a dramatic increase in heroin use.
Abusers of OxyContin were effectively faced with a decision: switch to heroin, use other opiates or get clean.
The decision, it turns out, was a generational one. According to Danita Sands, executive director and co-founder of Pathways Recovery in Placer County, two groups of addicts are currently seeking help, divided by both age and drug of choice.
The first group is made up of 18- to 30-year-old local heroin addicts who were in their teens and early 20s when the Oxycontin epidemic reached its peak. Heroin, for many of them, was an easy transition from OxyContin. It was the same high, but much cheaper.
“Prior to 2010, most of the young people we had coming here to detox were for OxyContin,” says Sands. “Now, it’s primarily heroin.” The second group is made up of the 30-and-over crowd. This group, according to Sands, is made up of soccer moms, executives, business owners — people who wouldn’t traditionally fit the stereotype of a “drug addict.” Rather than heroin, this group has moved onto other prescription opiates, avoiding heroin due to the stigma their generation associates with the drug.
“With the older clients, we see a lot of addiction to Vicodin, Norco, Percocet, Opana — lower strength medications than Oxycontin but just as powerful when taken in excess,” Sands states.
In Sands’ experience at Pathways Recovery, compared to the over-30 crowd, heroin doesn’t seem to carry the same stigma of being a “junkie” drug for the younger generation. Instead of OxyContin being brought down to the level of heroin, heroin has instead, for those under 30, been elevated to the level of OxyContin.
And that demand for heroin in the foothills is one that cartels from Mexico have been happy to fill.
“This is a new issue for affluent communities,” Sands explains, “where you have parents who are wealthy enough to not notice when money goes missing.”
Affluent communities like Folsom, where police have recently declared heroin the No. 1 drug problem.
Affluent communities like Roseville, where a heroin ring was recently broken up and whose court documents show heroin presence in Loomis, Auburn, Lincoln and Rocklin.
Dr. Andrew Kolodny, chief medical officer at the Phoenix House Rehabilitation Clinic, calls the heroin resurgence “the worst epidemic this country has ever faced.” In 2011, the federal Centers for Disease Control and Prevention declared opiate addiction an epidemic.
Thor Cain, an Auburn paramedic and EMT, says that drug-seeking 911 “emergency” calls from people who demand opiate medications “have gone from maybe three or four a month to at least one per day.”
And a 2014 survey of every pharmacy in Auburn found that hydrocodone, a powerful synthetic opiate, was the most-prescribed medication.
Opiate addiction is here. Heroin addiction is here. At this point, that is indisputable.
In 2010, the CDC reported that “enough [opioid painkillers] were sold to medicate every American adult with a typical dose of 5 milligrams of hydrocodone every four hours for one month.”
With only 5 percent of the world’s population, the U.S. consumes 80 percent of its opiate supply.
Charmaine Moller, an Auburn pharmacist for the past 10 years, has seen the dramatic increase in opiates in Auburn firsthand.
“These doctors aren’t treating the problem. They’re treating the symptom and handing out these medications,” she explains. “Not all doctors. But it only takes a few who hand out pills like candy, and pretty soon people are hooked.”
Deputy Poiesz offers a more complete picture: “The pill user of yesterday is the syringe user of today. That whole demographic that we used to bust with prescription drugs a few years ago, now have track marks on their arms from needles,” he says. “And they all started by saying they’d never switch to heroin. But at some point, it became inevitable.”
As for Auburn’s future, Poiesz pauses and lets the question settle. “I wish I could say there’s a positive light at the end of the tunnel, but it’s hard to say,” he says, his voice drifting off.
“We’re definitely facing an uphill battle.”
In December 2012, the year after the CDC declared an opiate epidemic in America, a company in California submitted its application to the FDA’s Anesthesia, Analgesia and Addiction Products section.
The application was to market Zohydro, a new, high-dose, long-acting pain medication. The drug was submitted in capsule form, with no effort made to make it tamper-resistant.
In a familiar tone, the makers of the drug extolled the benefit of the powerful narcotic, explaining how the drug needed to be taken only once or twice a day, compared with the every 4-6 hours of existing hydrocodone tablets.
At the public hearing, parents and families whose lives were destroyed by addiction that began with prescription drug abuse lined up to speak, practically begging the panel to reject the drug’s application.
The FDA’s scientific advisory committee, made up of doctors and researchers responsible for safety recommendations, which the FDA almost always follows, voted 11-2 to reject the drug.
In October 2013, the FDA approved the high-dose, non tamper-proof version of Zohydro.
“The benefits,” the FDA declared in a statement, “outweigh its risks.”
Part 3: To Hell and Back
It really is a shame that the last image I have of my Uncle Mark is him lying on the floor, dying, with my left hand behind his head and my right hand under his chin, trying to somehow breathe my life into him. A syringe lay at his right, a burnt spoon on the table, empty Saran Wrap and a lighter on the floor. Just chaos. Uncle Mark was a gracious man, and part of me feels like he deserved a better final mental snapshot than that.
I was 13.
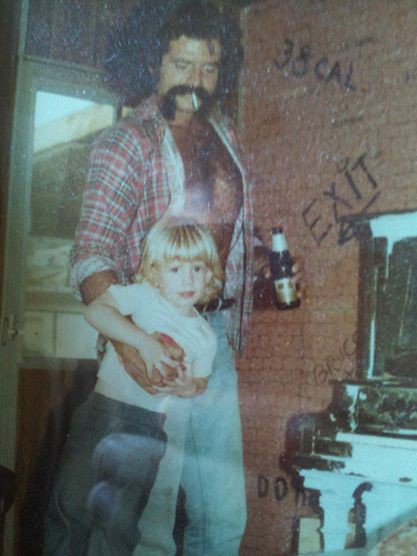
image provided by Jason Smith
Uncle Mark was 39, and he knew he had a problem. He had used heroin since he was 14, so that was undeniable. But admitting he had a problem was something he refused to do.
Knowing something comes from one’s head. Admitting it comes from one’s heart. And he’d lost touch with his heart well before he lay dying in my arms.
Heroin eats away at your soul, at that intrinsic little voice that tells us right from wrong, good from bad, love from hate. It numbs everything in its path; the soul is just an innocent bystander.
It takes everything you love, everything you care about, all of your dreams, your aspirations, your friends, your family, everything — and pushes it to the side in favor of finding ways and means to get more heroin.
And until an addict finally succumbs to reality and admits he or she has a problem, there can be no solution. Sure, it can be forced. But more often than not, for addicts’ families, it’s nothing but a lesson in redundancy and heartbreak. It’s feeling stupid for actually believing they’d get it this time around. It’s wondering what they did wrong and how they could’ve stopped such a beautiful person from taking such an ugly path through life.
For the addict in denial, it’s promises — lots and lots of empty promises. Nothing kills the soul more than failing, once again, like they said you would. Nothing annihilates your self-esteem more than using against your own will, possessed by an obsession to outrun a detox in $20 increments.
After the admission, solutions are plentiful. Help is out there.
Auburn, Grass Valley, Placerville, Rocklin and Roseville all have inpatient and outpatient rehabilitation services. County funding is available. There are 12-step meetings for both drugs and alcohol at nearly every hour of the day. Transitional living facilities are available for social reintegration.
The help is out there. But before we can receive it, we must first, as a community, admit that we have a problem. There’s no magic pill we can take to defeat addiction. And let’s face it — America being America, if there were a magic pill, we’d chop it up and snort it or find a way to smoke it on foil.
I spent about six weeks conducting interviews and research for this series. I wish I could say that the subjects were difficult to find — that there was only one drug dealer in town, that there was only one heroin addict in town, that there was only one person whose husband chose drugs over his own family. But the truth is that I was granted only so much space in this newspaper, and it wasn’t nearly enough.
There’s the story of a mother and father who dearly miss their daughter who went from being a straight-A college student holding down two jobs to living in a car in the course of 10 months because of her heroin addiction. A handful of ER nurses told me that their jobs are being constantly interrupted by waves of addicts trying to score narcotics.
The stories were plentiful, and they came from your friends and neighbors right here in Auburn.
If nothing else comes from this series, I hope a dialogue emerges. All of us have either a family member or friend who is battling addiction of one kind or another, and to convince ourselves that because we live in a tight-knit, upper-middle-class community we are immune to stereotypically “inner-city problems” is not only foolish; it’s dangerous. To put it more plainly: It’s denial.
Addiction doesn’t care how old you are, what color you are, what you do for a living, what kind of car you drive, what tax bracket you’re in, how much you love your husband or wife, how much you love your kids.
And it certainly doesn’t care that you live in Auburn.
The isolation of living in the foothills didn’t protect Kristin Netto (Thursday, Part 1) from having her life torn apart by her husband’s drug addiction. Her little boy is now three years old, and when he asks for his father, her only response is, “Daddy’s still sick,” she explains. “What else do you tell a three-year-old?”
She has since filed for legal separation, receiving full custody of not only her biological son, but also her soon-to-be ex-husband’s two sons from a previous relationship. As of the writing of this article, he’s still disappeared into his addiction.
The drug dealer (Part 1), “Kevin,” is trying to stay clean. “When I’m clean, I don’t sell,” he says. “I don’t need to.” At the writing of this article, he was two days clean. That may not sound like much, but believe me, two days clean for a drug addict is two consecutive 24-hour miracles.
As for “Michael” (Part 1), after completing the Community Recovery Resources program in Grass Valley, he has been clean for 42 days. He’s just 19 years old, and the temptation of old friends carries with it the temptation of old habits. To say he has an uphill battle in front of him would be an understatement, but to say it’s an impossible task would be to sell short the human spirit. Millions of others have done it, and it’s up to him to decide whether he is finished. I wish both “Kevin” and “Michael” nothing but the best.
As for me, my clean date is irrelevant, but let’s just say I know what the road ahead of them looks like. I’ve been there. I am there. It’s difficult and it’s trying and it’s frustrating and it’s probably the most beautiful, rewarding journey of self-discovery one could ever embark upon.
You’d think that holding my uncle while he took his last breath would’ve scared me away from ever touching drugs.
You’d be wrong.
It doesn’t work that way. It’d be nice if it did, because then we could show kids “Scared Straight” videos, show them an egg frying in a pan and tell them that “this is your brain on drugs,” come up with catch slogans like “Just say no!,” and we’d never have to worry about them trying drugs.
How has that worked out so far?
No, my path to hell went the prescription drug route after having a back surgery, and when I went in, I went in deep. I almost didn’t make it out. In fact, for all intents and purposes I shouldn’t have, at least according to the ER doctors. But I did, and now I feel that I have an obligation to make the most of this second chance by doing what I can to give back.
Don’t get me wrong; it’s hard work. For me it requires a healthy dose of 12-step meetings, lots of sponsoring, going into rehabs to speak, letting people know there’s a better life awaiting them should they choose to live it.
Addiction does not have to be a dead end. There is a way out. You just have to be ready to find it.
If you had just met me on the street, you’d probably never know that I was a recovering addict.
You’d never know that I’ve seen hell up close and personal, all over the world, in multiple languages, in a variety of cultures, and I didn’t know whether I had what it took to make it back.
You’d never know unless I was willing to talk about it. ![]()
All Cut Up Films has received the film rights to Heroin In The Foothills and Bitter Taste of Dying (short film).